DDX of papilledema
Papilledema refers to optic disc swelling that is commonly related to increase intracranial pressure. Causes of intracranial pressure are:
- Intracranial mass lesions (e.g. tumor, hematoma)
- Cerebral edema (hypoxic-ischemic encephalopathy, large cerebral infarction, severe TBI)
- Increased CSF production (choroid plexus papilloma)
- Decreased CSF absorption (arachnoid granulation adhesions)
- Obstructive hydrocephalus
- Obstruction of venous outflow (venous thrombosis, jugular vein compression, neck surgery)
- Idiopathic intracranial hypertension (psuedotumor cerebri)
Patients commonly complain of headaches, transient visual disturbances that occur in one eye (unilateral) or both eyes (bilateral). Visual acuity is not affected unless the papilledema is severe, chronic, and patient also has macular edema and hemorrhage. Visual field tests would show enlarged blind spots and peripheral constriction. Additionally with psuedotumor cerebri, most patients are obese females. Treatment includes weight loss, and acutely with carbonic anhydrase inhibitor such as acetazolamide to lower ICP, however further treatment of increased ICP is specific to underlying cause.
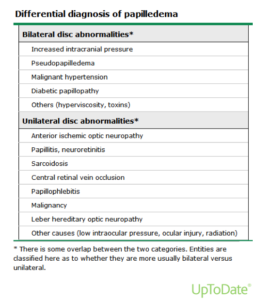
Differential of papilledema include:
Reference:
- Chumley HS. Papilledema. In: Usatine RP, Smith MA, Mayeaux, Jr. EJ, Chumley HS. eds. The Color Atlas and Synopsis of Family Medicine, 3e New York, NY: McGraw-Hill;http://accessmedicine.mhmedical.com.york.ezproxy.cuny.edu/content.aspx?bookid=2547§ionid=206777859. Accessed April 17, 2020.
- Horton JC. Disorders of the Eye. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J. eds. Harrison’s Principles of Internal Medicine, 20e New York, NY: McGraw-Hill; . http://accessmedicine.mhmedical.com.york.ezproxy.cuny.edu/content.aspx?bookid=2129§ionid=192011900. Accessed April 17, 2020.
- https://www.uptodate.com/contents/overview-and-differential-diagnosis-of-papilledema?search=papilledema&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
Tumor markers CA-125 and CEA
A tumor marker can be proteins or other substances that are produced by cancer cells or other cells of the body in response to cancerous or benign conditions. These marker can be found in blood, urine, stool, tumors, and such of patients with cancer. However when elevated these markers are nonspecific since it may be present in benign conditions or even with liver or renal disease. So results should be interpreted with caution, as they may not be helpful in determining the primary tumor site.
There exists many different tumor markers that are associated with one type or multiple cancer types. But they are not 100% sensitive and negative markers cannot be used to rule out possible cancers. There are two main types of tumor markers: circulating tumor markers and tumor tissue markers.
Circulating tumor markers are found in blood, urine, stool, and other bodily fluids. This type is mainly used to estimate prognosis, detect residual cancer or reoccurrence after treatment, the response to treatment interventions, and if the cancer has become resistant to treatment.
Tumor tissue markers are located in actual tumors from a sample during a biopsy. These markers are used to diagnose, stage, and classify the cancer; estimate prognosis; help to select appropriate treatments.
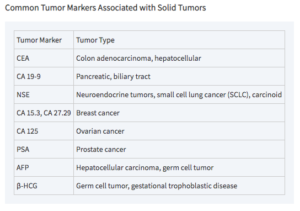
A couple or tumor markers are the CA-125 and CEA that are used in the aid of diagnosing cancer and targeted for therapy. The CA-125 marker is obtained from blood samples, and is closely associated ovarian cancer. They utilize this marker to aid in diagnosis, assessment of response to treatment, and evaluation of reoccurrence. The CEA tumor marker or Carcinoembryonic antigen is also analyzed in the blood, and is related to colorectal cancer and some other cancers such as pancreatic, gastric and breast. This marker is largely used to keep track of how well cancer treatments are working and to check if it has reoccurred or spread. Other tumor markers are summarized in the following chart.
Sources:
- Varadhachary GR, Abbruzzese JL. Carcinoma of Unknown Primary. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J. eds. Harrison’s Principles of Internal Medicine, 20e New York, NY: McGraw-Hill; . http://accessmedicine.mhmedical.com.york.ezproxy.cuny.edu/content.aspx?bookid=2129§ionid=192016706. Accessed April 18, 2020.
- https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-fact-sheet#what-tumor-markers-are-currently-being-used-and-for-which-cancer-types
- https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list