Pharmacology Case Discussion #1- Prof. County Online Clinical Rotation
D.S. is a 65-year-old white woman, who implemented lifestyle modifications for her dyslipidemia 6 months prior to her follow-up clinic visit last December. She has a Hx of gout, chronic nonischemic HF (LVEF 28%), and diabetes (diet controlled) as well as a 20 pack-year smoking history (quit 5 years ago).
Her medications included lisinopril, furosemide, metoprolol succinate 25 mg Once Daily.
Her vital signs included BP 124/80 mm Hg, and HR 75 beats/minute. Her laboratory results were as follows: HDL-C 64 mg/dL, LDL-C 101 mg/dL, TG 98 mg/dL, and TC 185 mg/dL.
Discuss the appropriate next step for pharmacologic management of D.S’. dyslipidemia, along with pharmacologic agents for her comorbidities.
- Please briefly justify/explain your choice/s of pharmacologic agent/s (Please include the complete regimen).
In this case scenario, in order to properly treat her dyslipidemia, we would first obtains Ms. D.S.’s risk for atherosclerotic cardiovascular disease (ASCVD) and then recommend management strategies.
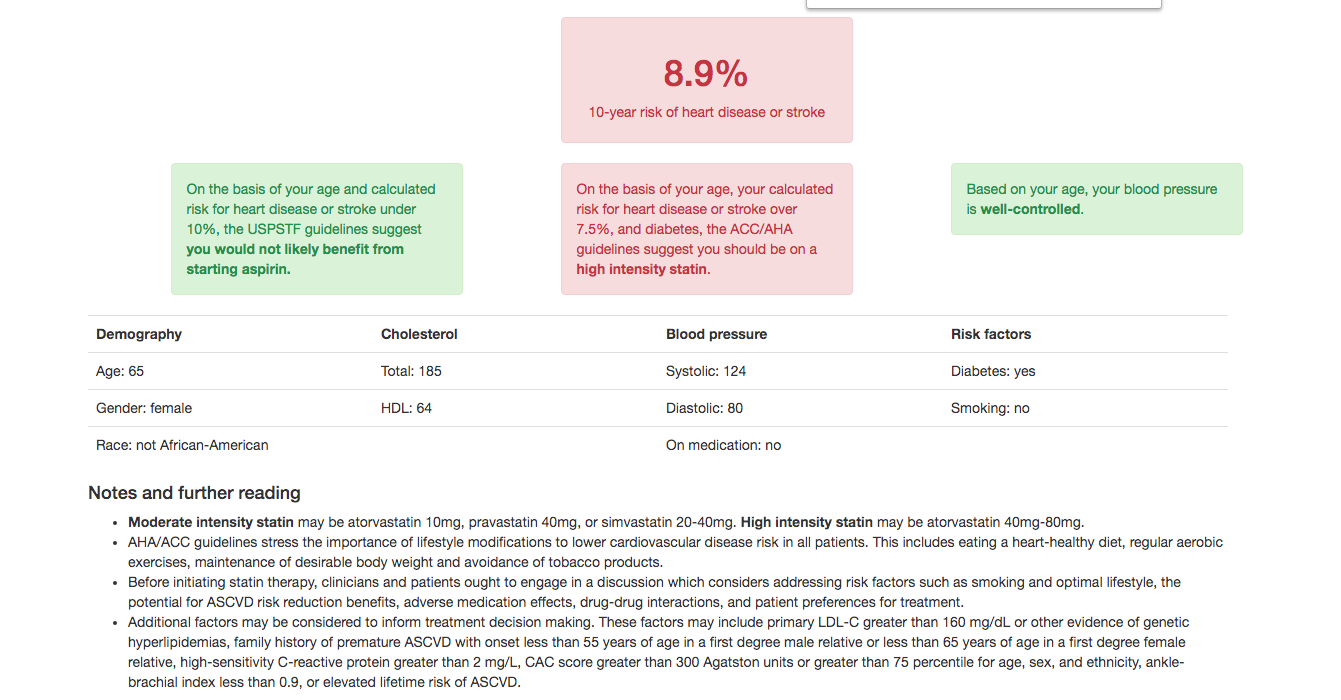
Heart Risk Calculator
According to her ASCVD risk estimation, the 10-yr risk of heart disease or stroke is 8.9%. Ms. D.S.’s blood pressure is well controlled and since her risk is under 10% a low dose aspirin would not be beneficial at this time. According to her ASCVD risk estimation, and the ACC/AHA guideline, she should be placed on a high intensity statin such as Atorvastatin 40-80 mg or Rosuvastin 20-40 mg.
In this case I would start Ms. D.S. on Atorvastatin 40 mg and assess her adherence, response to therapy, and adverse effects within 4 to 12 weeks following statin initiation; especially since combo with some beta blockers (metoprolol) may decrease antihyperlidemic efficacy. Although her labs indicate that her lipid profile is only slightly elevated, she is recommended to start on a high intensity statin for primary prevention of ASCVD primarily due to her age and history of diabetes mellitus. Starting on a statin is the most effective agent for lowering LDL, it may increase HDL, and lower triglycerides. Additionally prior to starting statin therapy a baseline serum creatine kinase (CK), TSH, and LFTs should be obtained for possible future reference.
Ms. D.S. should also be educated on a healthy diet that consists of vegetable, fruits, nuts, whole grains, animal protein, fish, while minimizing intake of trans fat, red meat, processed meats, refined carbohydrates, and sweetened beverages. She should also be counseled physical activity and exercise recommendations.
As for her other comorbidities she should continue her lisinopril, furosemide, metoprolol succinate 25 mg once daily as prescribed unless she complains of any side effects.
Today (4/7/2020), four months later, D.S. is admitted to the hospital with atrial fibrillation, which she said began 1 week ago “occurring off and on several times daily”. On physical examination, she was found to have rales; her extremities have 2+ pitting edema. ECG showed a ventricular heart rate of 140 beats/min.
Discuss the pharmacologic management of A. Fib, along with pharmacologic agents for her comorbidities.
- Please briefly justify/explain your choice of pharmacologic agent/s (Please include the complete regimen).
During this hospital admission Ms. D.S. is found to have AF and on PE she had rales, 2+ pitting edema. Given her PMHx this indicates she may be experiencing an acute decompensating heart failure and such her AF can be a result of her acute HF due to increases in left atrial pressure and wall stress. She should be placed on cardiac monitor, IV access, and supplemental O2 if indicated by her vitals. I would order a portable CXR, and bedside Echocardiography. Labs to obtain are CBC, CMP, troponin, ABG if she is in respiratory distress, LFTs, BNP, PT, PTT, and INR.
With the new onset of AF, you can calculate her thromboembolic event/stroke risk with the CHA₂DS₂-VASc Score. I obtained a score of 4, due to her age, sex, CHF history, and Diabetes mellitus history. This indicates she is at moderate-high risk, and should be on anticoagulation, such as warfarin or non-vitamin K antagonist oral anticoagulant (NOAC). Her risk of ischemic stroke is 4.8% per year, and 6.7% risk of stroke/TIA/systemic embolism.
Medical Treatment/Management at admission
- Beta-blocker should be held in decompensated HF due to its negative inotropic properties, which can worsen her clinical condition. It can be restarted once she is stabilized.
- Give IV Furosemide 40 mg bolus for volume overload – It should equal to or greater than her current maintenance total daily oral dose.
- Monitor: Volume status, electrolytes, and renal function
- Consider Sodium and fluid restriction
- Give IV Amiodarone 150mg over 10 mins, then 1mg/min x 6H, then 0.5mg/min x18H for rate/rhythm control – it has very little negative inotropic activity and usually more effective than Digoxin to slow heart rate
- Initiate PO Rivaroxaban 20mg daily for thromboembolism/stroke prophylaxis – compared to warfarin it has a high efficacy in preventing stroke in AF, lower incidence of major bleeding, once a day dosing, minor drug and food interactions, predictable PK and PD, rapid onset and offset of action, short half-life, and no need for constant laboratory monitoring.
- Refer to Cardiology upon discharge
Overall Drug Profile
- Atorvastatin 40 mg
- Lisinopril as prescribed
- Furosemide as prescribed
- Metoprolol succinate ER 25 mg
- Amiodarone 200 mg
- Rivaroxaban 20 mg
Recap of major points discussed today:
- ASCVD Risk calculation for selecting appropriate therapy for your patient’s dyslipidemia.
- Management of your patient’s atrial fibrillation on admission to the hospital (Rate control/Thrombus prophylaxis/Rhythm control)
- Discharge medication/s for atrial fibrillation
- Review of your patients overall drug profile
Sources:
- https://www.ahajournals.org/doi/pdf/10.1161/CIR.0000000000000677
- http://www.cvriskcalculator.com/calculated?age=65&gender=0&race=0&total-chol=185&hdl=64&sbp=124&dbp=80&treated=0&diabetes=1&smoker=0
- https://www.uptodate.com/contents/treatment-of-acute-decompensated-heart-failure-components-of-therapy
- https://www.uptodate.com/contents/the-management-of-atrial-fibrillation-in-patients-with-heart-failure
- https://www.mdcalc.com/cha2ds2-vasc-score-atrial-fibrillation-stroke-risk
- https://www.uptodate.com/contents/prevention-of-venous-thromboembolic-disease-in-acutely-ill-hospitalized-medical-adults
- https://www.uptodate.com/contents/atrial-fibrillation-anticoagulant-therapy-to-prevent-thromboembolism