Chapter 19
Case study
Ms. S is a 35-year-old woman who comes to the outpatient clinic for an initial visit. She is well and is without complaints. On review of systems, she notes that she occasionally passes bright red blood per rectum. This has happened about 4 times over the past 5 years. It is never associated with pain. She sometimes sees the blood on the toilet paper and sometimes in the bowl.
On further history Ms. S reports no recent change in bowel habits, no weight loss, and says she feels well. She does report that although the bleeding has never been associated with pain, it is sometimes associated with constipation. She has never used any treatment.
Ms. S has a normal general physical exam. External anal exam and digital rectal exam are normal. Anoscopy reveals 1 large, non-33bleeding internal hemorrhoid. A CBC is normal.
One year later Ms. S returns to the clinic with recurrent bleeding. Anoscopy revealed a bleeding internal hemorrhoid. Symptoms resolve with supportive care, but bleeding recurs 1 month later. Colonoscopy is performed and reveals only internal hemorrhoids. The patient declines definitive therapy and continues to experience rare episodes of hemorrhoidal bleeding.
SOAP NOTE
S: 35 y/o female who presents to initial appointment w/ no complaints, however states she passes bright red blood per rectum x 4 over 5 years. She states that she notices the blood on the toilet paper and sometimes in the toilet bowl. Patient states it is never associated with pain but sometimes with constipation. Has not taken anything to relieve symptoms.
O: Patient is a well developed female and looks her age, good hygiene and well groomed, in no apparent acute distress,. Physical exam, unremarkable. External anal exam, unremarkable. Digital rectal exam, unremarkable. Laboratory results CBC, unremarkable. Anoscopy reveled 1 large nonbleeding internal hemorrhoid.
A: Internal Hemorrhoids
R/O Anal Fissures
P: Educate patient on diet to include more high fiber rich food such as fruits and vegetables, or to use fiber supplements to prevent constipation. Increase fluid intake, follow up if symptoms worsen or do not improve. Speak to patient about possible surgery for removal.
Summary
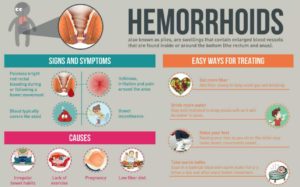
When a patient presents with GI bleeding, red flags to consider include anemia, change in bowel habits, weight loss, and diarrhea. Differential diagnoses to consider with GI bleeding are: Hemorrhoids, Anal fissures, which presents with bright red blood per rectum, often associated with pain and diagnosed with internal inspection or Anoscopy; Ulcerative Colitis, which is associated with diarrhea and Colon cancer, they would have a history of anemia, change in bowel movements, or family history of colon cancer, these are diagnosed with a colonoscopy.
Hemorrhoids are classified as either internal or external. Patients with hemorrhoids have recurrent flares. Treatment for hemorrhoids and anal fissures can be conservative with recommendation of perianal wellbeing. Recommendations include a Sitz bath to relax the anal sphincter, acetaminophen, topical exams, or topical corticosteroids. A doughnut shaped cushion is also recommended for prolong sitting. Increase fluid intake and a high fiber diet, or mineral oil. Avoid prolong sitting, especially on the toilet and constipation. Internal hemmorids may continue to bleed and may require surgical removal. If the hemorrhoid is irreducible or thrombosed it will require rapid surgical treatment.